AMCP Precision Medicine Partnership Forum: 5 Key Takeaways

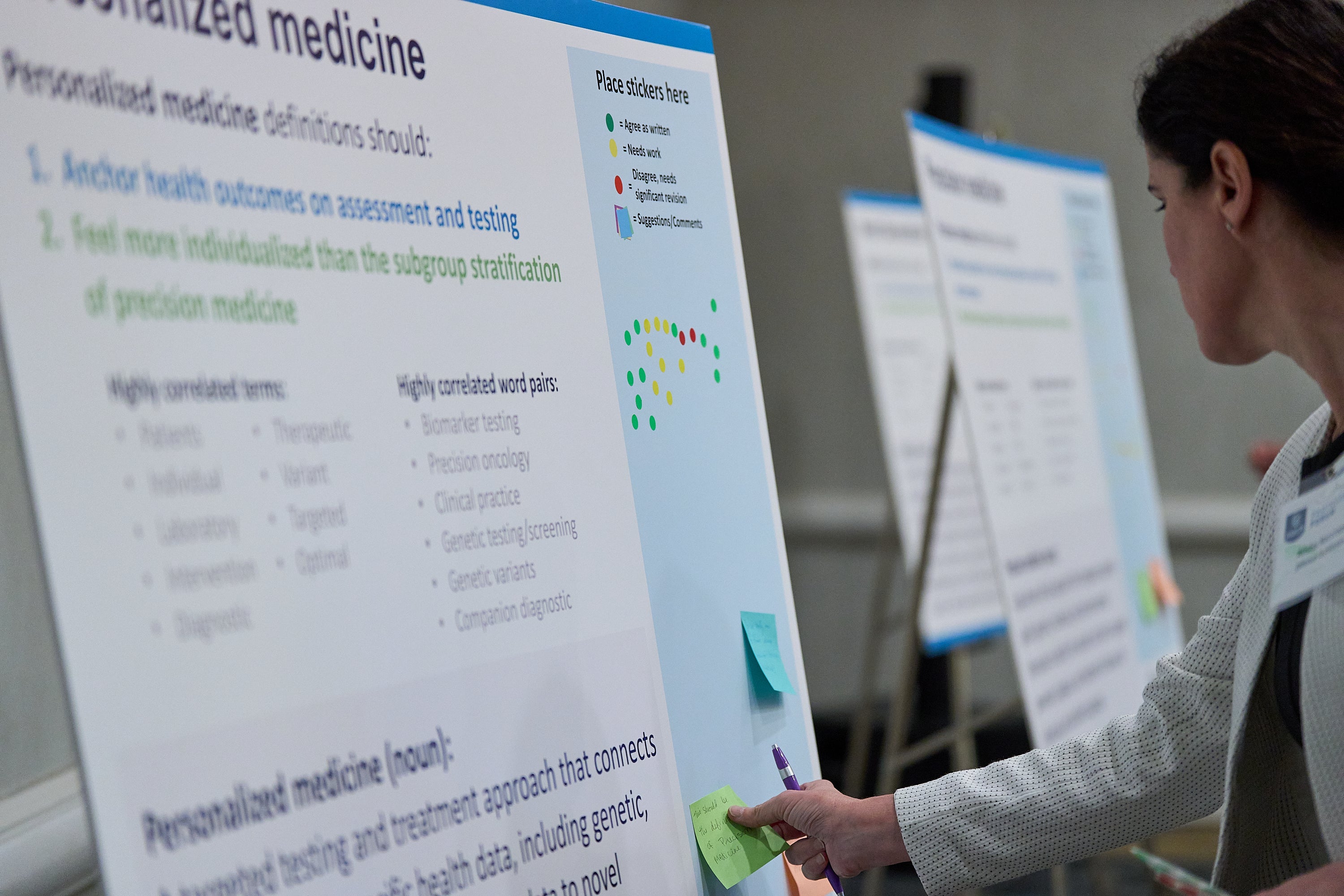
In June, AMCP convened leading experts from across health care disciplines for a two-day Precision Medicine Partnership Forum. The forum aimed to advance equitable and timely access to precision medicine, particularly in oncology. To see who presented and participated, view the program guide.
High-impact gaps and actionable solutions to address them were identified around prioritized topics including:
Understanding barriers and pitfalls that a patient experiences throughout the biomarker testing journey:
- Recognizing the patient’s journey through cancer care exposes how health system barriers create life-or-death consequences, highlighting the need to make patient voices central in policy decisions, streamline testing workflows, and prioritize equitable, timely access to precision-medicine tools.
- Only by aligning coverage, clinical guidelines, and care coordination around real-world experiences can managed care stakeholders truly improve patient-centered outcomes.
Review the current landscape of precision medicine:
- Access barriers to both biomarker testing and targeted treatments continue to persist. Coordinated solutions such as expanding biomarker testing coverage and dismantling downstream payment obstacles are essential next steps to address this issue.
- Clinicians face operational complexity once a precision therapy comes to market. Clear, actionable guidance on who and when to test, which assay to order, and how to interpret results is critical. Sustainable progress hinges on simplifying workflows and reducing the current system’s complexity.
Align clinical guidelines with coverage decisions:
- Guideline concordance has been shown to improve survival, equity, and value, yet payer policies still vary dramatically by disease stage and lab provider. Misalignment with guidelines creates coverage gaps and inconsistent access to essential biomarker tests and targeted therapies.
- Persistent external barriers, such as high drug costs and rebate-driven coverage, lead to guideline discordance. This necessitates ongoing collaboration between payers, clinicians, and NCCN to refine preference designations and ensure real-world adherence, ultimately increasing patient access to diagnostic testing and improving health outcomes.

Promote reflex (pathologist-initiated) biomarker testing protocols to streamline diagnosis:
- Pathologists serve as the critical gatekeepers for precision oncology but are often insufficiently integrated into care teams. Empowering them to initiate comprehensive molecular testing at diagnosis can streamline workflows, reduce delays, and mitigate bias.
- Overcoming barriers requires multidisciplinary solutions to embed test orders in pathology workflows, leverage nurse or lab navigators for insurance verification and result coordination, and deploy EHR alerts to keep oncologists informed.
- Piloting pathologist-initiated testing protocols across varied institutions—and co-designing implementation guides with pathology and oncology societies—will accelerate widespread adoption, ensuring timely, accurate diagnostics and targeted treatment for every patient.
- Early modeling of pathologist-initiated testing protocols across diverse sites will accelerate widespread adoption and ensure timely, accurate diagnostics and targeted treatment for patients. Coordination with pathology and oncology organizations is essential to produce actionable implementation guides for broader adoption.
Define clinical utility to support appropriate test use and treatment selection:
- In precision oncology, clinical utility is determined by a test's demonstrated impact on meaningful patient outcomes, but there is ongoing debate over which outcomes should be prioritized.
- Rather than a one-size-fits-all definition, stakeholders decided to achieve consensus on a core set of parameters while allowing flexibility to select endpoints based on clinical context.
- Effective implementation requires clear separation of diagnostic versus treatment policies, standardizing workflows, and enabling payers to assess utility before cost.
Other key discussions included generating robust real-world evidence and addressing inconsistencies in interpreting the 14-day rule. Aligning payers, providers, and patients on these issues will promote more consistent, value-driven access to biomarker testing.
AMCP would like to thank Forum Participants and Valuate Health Consultancy for their contributions to the Partnership Forum and commitment to improving precision medicine management.
View Program Guide View Takeaways PDF
AMCP Precision Medicine Initiative

Mitzi Wasik
SVP, Practice Strategy & Innovation
& AMCP Foundation Executive Director
Published on July 31, 2025
Featured News & Resources
See Full CalendarUpcoming Events
AMCP offers a wide variety of educational opportunities, from events and webinars to online training.